| HOME | SPINAL CONDITIONS | PROCEDURES | CLINICS | BACKGROUND | CONTACT | MEDICO-LEGAL |
Spinal Conditions |
|
Spinal conditions managed include neck pain to back pain, disc prolapse, spinal stenosis, spondylolisthesis, whiplash, sports injuries (including spondylolysis and stingers), scoliosis, adult spinal deformity, spinal tumours and infection, spinal surgery for rheumatoid arthritis and spinal trauma. List of ConditionsClick on a heading below to find out more. AnatomyBack PainDegenerative Disc DiseaseDisc Prolapse (Prolapsed Intervertebral Lumbar Disc – Sciatica)Spinal Stenosis (Spinal Claudication)SpondylolisthesisProlapsed Intravertebral Cervical DiscsSciaticaFacet Joint SyndromeSpinal TraumaSports InjuriesStingersSpinal TumoursScoliosisSpinal Kyphotic DeformityRheumatoid Arthritic Spinal DiseaseCoccydynia (pain around the coccyx)Sacroiliac Pain |
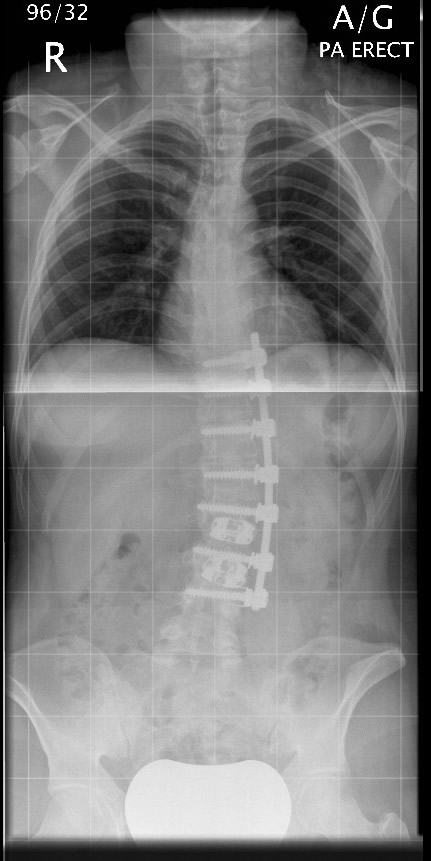
AnatomyThe spinal column extends from the skull to the pelvis, there are 33 individual spinal vertebrae, which are stacked in a column separated by discs which act as shock absorbers. The vertebrae are linked posteriorly (at the back) by facet joints. Strong ligaments and muscles support the spine and provide flexibility and movement. The spinal cord and nerve roots allow passage of messages from the brain to other areas of the body including muscles of the arm and legs. The spinal column, including the nerves, muscles and joints all should work in harmony to allow stability and movement. 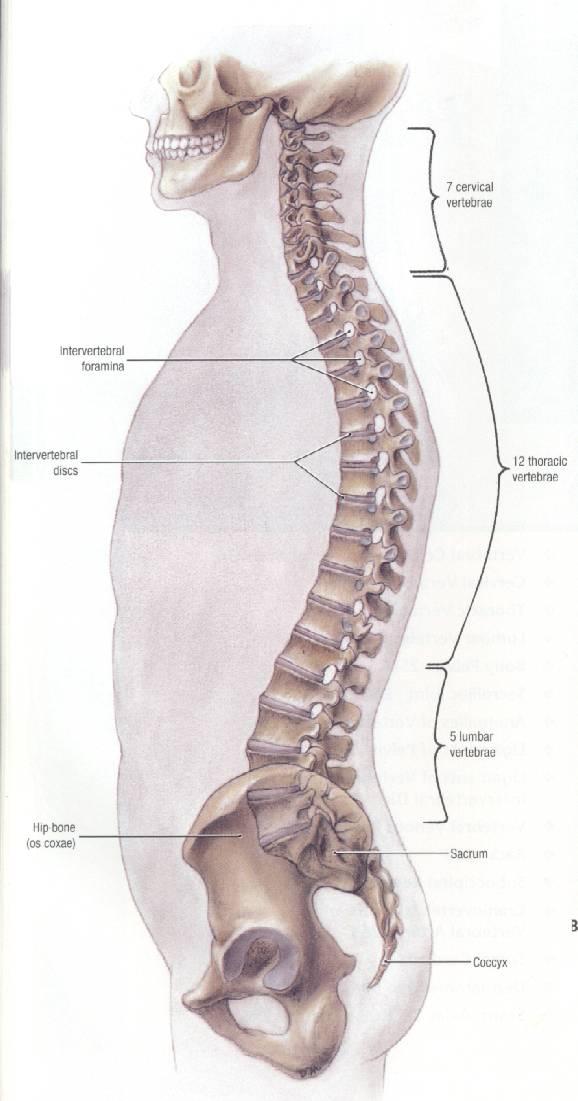
The spine offers protection to the spinal cord and has four gentle curves from the side view (sagittal profile) which supports the head above the pelvis allowing optimal muscle function. 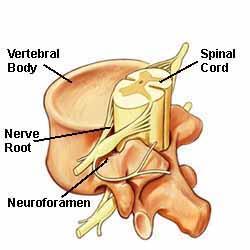
Back PainBack pain is very common and most of us will have symptoms at some time in our life. It is recognised that increased sedentary occupations lead to increased episodes of back pain. Occupations such as office work can involve up to 40 hours in a static position at a desk. Commuting to and from work also includes sitting or standing depending on the transport. Evenings usually involve sitting for dinner or in front of the TV as opposed to exercise programmes. To encourage a healthy back, it is important to keep the back moving and to exercise the supporting structure. Try to enable good posture without slumping while standing and sitting. Strengthening your back muscles and keeping fit is important and walking on flat and inclines encourages aerobic activity and swimming is an excellent exercise. Some people need to avoid breast stroke which can strain your neck. Take care when lifting and bend your knees if possible and not your back. Keep you feet shoulder width apart as this gives stability to the spine. Always carry objects close to your body so that this shifts the centre of gravity towards you. If you are unlucky enough to have an attack of back pain, do not rest for any more than three days. You will not do your back any harm by moving around, even if it is uncomfortable. You will probably recuperate more quickly if you keep active. Try to return to your normal activities as soon as possible and continue as your pain allows, therefore it is important to pace yourself. Keeping fit and strengthening your back muscles is very important including core stability. Back pain may be acute or chronic, acute episodes last less than six weeks but chronic episodes persist. Long term pain can last a life time. Patients who have chronic pain can have acute episodes intermittently over the years. Back pain can cause a sudden and sharp pain or a dull toothache type of pain. Pain can occur with movement, such as sneezing or coughing. You may develop pain or numbness in your arms and legs (leg symptoms referred to as sciatica due to nerve irritation). It is important to treat your back correctly (seek medical attention if back pain persists). Symptoms suggestive of requiring medical attention include:
One of the causes of low back pain can include spinal stenosis, facet joint arthritis, osteomyelitis and discitis (spinal disc infection), tumours (benign and malignant), spondylolisthesis and vertebral fractures as a result of trauma or osteoporosis. Degenerative Disc DiseaseDegenerative disc disease can occur in people as young as twenty. Usually it affects the older age group and is part of the natural wear and tear of a normal aging spine. If you have chronic back or neck pain, you may have degenerative disc disease. As the spine ages, the intervertebral discs between the vertebrae lose their flexibility, elasticity and ability to act as shock absorbers. As a disc loses it’s suppleness, the spine becomes more rigid and stiff and patient’s tend to lose movement. Degenerative disc disease can affect any part of the spine and usually occurs in areas of movement, mainly in the cervical (neck) and lumbar (low back) spine. Patients can present with either lower back or neck pain but quite often have a combination of both depending on where the degenerative disc disease causes symptoms. Symptoms can be worse when sitting, bending and lifting with less pain when lying or walking. You should seek treatment if pain becomes worse and is disabling. Any signs of arm or leg weakness or numbness and especially any alteration in bladder or bowel control. Back pain is not always a sign of degenerative disc disease and therefore treatment is focussed on the cause of the symptoms. Disc Prolapse (Prolapsed Intervertebral Lumbar Disc – Sciatica)As the disc ages, it loses it’s flexibility and water content, which can be related to inherited factors, previous injury, smoking and occupation. The disc itself does not slip but the outer thick wall (annulus fibrosis) splits or ruptures. Following this the inner gel like material (nucleus pulposus) leaks out. This is termed a disc herniation and people between the ages of thirty and fifty are at most risk of this due to the reduced elasticity of the nucleus pulposus. Disc herniation may only cause back pain but depending on the site and size of the herniation it can press against a nerve leading to nerve root irritation and if this occurs in the lower back, it can give rise to a condition known as sciatica. The nerve that is irritated is one of the nerves that forms the sciatic nerve and gives referred pain down the leg towards the shin, foot and ankle. Spinal Stenosis (Spinal Claudication)Spinal stenosis essentially means narrowing of the spinal canal through which the nerves travel down the spine and exit at each level to supply either the arms or legs. This most commonly occurs in the lower back (lumbar region) or in the upper neck (cervical region). There are several causes for this, including a congenital (inherited) cause or more commonly this occurs as the spine ages as the discs bulge into the canal along with thickening of the posterior ligaments (ligamentum flavum) and enlargement of the facet joints (hypertrophy). Even the vertebrae can through off bony spurs (osteophytes) that can also narrow the spinal canal. In some occasions the vertebrae may not sit upon each other correctly which can also narrow the spinal diameter (spondylolisthesis). Chronic symptoms arising from lumbar spinal canal stenosis are pain into both legs, with occasional weakness and numbness which can be felt in the buttocks, legs or calves. These symptoms tend to occur with walking and causes the patient to only walk shorter distances but then tends to improve as the patient bends forward or sits. This condition can be mistaken for vascular (arterial blood vessel) narrowing and occasionally is difficult to separate. Symptoms from cervical spinal canal stenosis may give rise to pain and weakness in the shoulders, arms and hands with alterations in hand function as well as stiffness in both legs. As the canal narrows it can lead on to bladder and bowel problems as well as paraplegia with the loss of ability to walk, but this is very rare. SpondylolisthesisSpondylolisthesis is a condition where one vertebra slips forward on the vertebra below it, this tends to occur in the lower lumbar spine and can be present from birth or develop as the spine ages. It is a reasonably common condition and can be the result of stress fractures to the posterior part of the spinal column, severe arthritis of the facet joints or following previous surgery. The degree of forward slippage can be graded from minimal to severe on a scale of one to five, Grade V is when the vertebrae is sitting in front of the one below. Prolapsed Intravertebral Cervical DiscsDisc prolapses can occur in the neck as a result of degenerative disc disease. The disc prolapse can cause pressure on the nerve running down the arm and this is called brachalgia (sciatica of the arm). Associated with the pain, you can have pins and needles or weakness in specific muscle groups and areas of the arm depending on the nerve involved. Of more concern in the cervical spine is possible compression on the spinal cord which can affect the arms and legs leading on to paraplegia. SciaticaSciatica results from pressure on a nerve in the lower back, which presents as mild to severe leg pain, this can be associated with weakness or numbness in the legs. This depends on which nerve is irritated and is most commonly related to a disc prolapse. It usually affects one side but can occasionally affect both. In some instances a very large disc prolapse can occur in the lower lumbar area which can press on the nerves to the bladder and bowel giving a condition called cauda equina syndrome, which requires immediate medical attention and treatment. Symptoms as a result of this condition include altered sensation around the anus, severe back and variable leg pain and loss of bladder or bowel control. Facet Joint SyndromeThere are a pair of facet joints, which are small joints at the back of the spinal canal. They are found throughout the length of the spine and therefore are present in the cervical, thoracic and lumbar spine. They allow movement and provide some stability. The facet joint is like a hip or a knee joint and can undergo arthritic change. As the disc narrows between the vertebrae, the facet joints will also wear and can give rise to a grating or clicking sensation as well as pain. Stiffness can be an early symptoms and can give rise to back pain which is worse when standing and lying and when leaning backwards. Spinal TraumaWhiplash is the commonest presentation of injury to the spine, commonly resulting from road traffic accident, sporting injury or an assault. Whiplash involves a strain to the soft tissues of the neck and upper part of the thoracic spine where the muscles and ligaments are stretched and bruised. Symptoms may commence immediately or develop over the next few days. Commonly pain around the neck and shoulders with some stiffness, but occasionally arm symptoms are seen involving some tingling or burning into the shoulders and arms. Sometimes if there is underlying degenerative disc disease and/or arthritis of the facet joints then symptoms can be proplonged. Injuries to the vertebrae themselves, require quite major forces, such as road traffic accidents, a fall from a height or as a result of sports injuries including rugby and horse riding. Fractures of the spine can occur throughout the spine from the cervical down to the lumbar spine, quite often stable but some do require expert evaluation and occasionally stabilisation due to the risks of spinal cord or permanent nerve impairment. Most nerve impairment occurs at the time of the injury and regrettably some of these injuries can be permanent. Another cause of fracture to the vertebrae involves osteoporosis which are termed fragility fractures. The vertebrae can collapse with minor trauma if the vertebrae is not as strong as it used to be. These fractures can be painful but rarely require any operative treatment. Some of these fractures can respond to insertion of cement. Sports InjuriesInjuries to the spine related to sport can occur during a specific injury (vertebral fracture or subluxation). Stress fractures can present due to repetitive loading (spondylolysis). Sporting injuries commonly involve the cervical spine and sometimes can result in spinal cord injury depending on the severity of the underlying injury. Sometimes emergency treatment is required if there has been mal-alignment of the spine. A common cause of back pain in young sporting individuals is a condition where there is stress fractures to the posterior aspect of the spinal column, namely spondylolysis. This is a reasonably common condition present in roughly 5% of the population. Obviously sports with increased extension to the lumbar spine can increase the risk of this. StingersThis commonly occurs with stretching of the upper part of the brachial plexus which is a group of nerves between the neck and the shoulder. The athlete/sportsman will complain of some burning pain with weakness in the arm. Spinal TumoursThese are fortunately rare but can present with similar symptoms to other more common spinal conditions. Symptoms can range from back pain, sciatica, numbness, scoliosis, night pain and fever. Commonest tumours arising in the spine spread from other areas in the body such as the breast, prostate, lung and kidney. They travel through the blood system to the spine and can go unnoticed until the vertebrae becomes weakened and back pain occurs. Sometime they can grow and press on the spinal cord leading on to weakness and paralysis. ScoliosisScoliosis, which is the term used for a spine with an abnormal rotatory curve, most commonly occurs in a growing spine in females. It affects approximately 2% of the population and can run in families. The spine has four natural curves looking at it from the side but doesn’t have a curve if you look at it from the front. It tends to be seen either early in the under 7’s or more commonly when the spine goes through it’s second growth spurt around the time of commencement of periods in girls. Shoulders can become unlevel and a fullnress seen over the back of the chest or loin area which is exaggerated by forward bending to touch their toes. Most scoliotic curves have little health impact, although some can become large and clearly visible which require monitoring and treatment. Scoliosis can occur in the older age group as a result of spinal degenerative processes. Sometimes an unnoticed scoliotic curve can progress in adulthood as opposed to commencing from a normal spine. Scoliotic curves in the adult can lead on to an increased instance of low back pain. Many scoliotic curves can now be restored to near normal and certainly progression can be abolished. Spinal Kyphotic DeformityThe most common spinal deformity is scoliosis as mentioned in a preceeding section. The spine has four natural curves looking at it from the side but one of these curves can become exaggerated and this is known as a kyphosis. It involves excess curvature in a forward direction and can result in a round or hunch back shoulder appearance. In the adolescent age, this can be as a result of an underlying developmental condition where some of the vertebrae can be wedged with abnormal adjoining discs and is termed Sheuermann’s disease. Kyphotic deformities can be either classified as postural, due to poor posture, which tends to improve when the patient is lying on their back or front or it is described as structural if this does not correct. Structural kyphosis can need medical attention if it is progressive and these curves tend to occur in the thoracic or thoracolumbar spine. Kyphotic deformities can be congenital where the vertebrae have not developed properly or can be associated with neuromusclular conditions as well as osteoporosis where you see several wedged vertebrae. Rheumatoid Arthritic Spinal DiseaseRheumatoid arthritis can affect the cervical spine in up to 90% of patients. This can result in neck pain, decreased range of movement as well as headaches. Neurological impairment can gradually occur, which shows up as weakness, decreased sensation. Rheumatoid arthritis can cause abnormal movement at the top of the cervical spine, namely atlanto-axial subluxation which can occur in 50-80% of cases. If this does occur then it can reduce the space available for the spinal cord. As well as this there can be some erosion and bone loss between the base of the skull and the upper part of the neck known as cranial settling. In the lower part of the neck, which occurs in up to 20% of rheumatoid cases, multiple disc degeneration and subluxations can be seen. Coccydynia (pain around the coccyx)This can result from a fall or can be of insidious onset. Patients tend to take to sitting on a ring to try and offload the painful area. Treatment involves anti-inflammatories as well as injection of local anaesthetic and steroid into the sacrococcygeal joint and very occasionally if this does not improve symptoms then the coccyx can be removed. This is a last resort and is associated with high complication and failure rate. Sacroiliac PainSome patients can get pain in the lower part of the back and also the buttock area from sacroiliac joint discomfort. This pain can arise from general arthritic conditions such as ankylosing spondylitis or can arise for no reason. If symptoms are resistant to analgesia and physiotherapy then an injection of local anaesthetic and steroid into the joint can assist in pain management. A last resort is to consider fusion of the joint. Before fusion is performed then X-rays with the patient standing on each leg is performed to show that there is no abnormal movement of each side of the pelvis. |
Design by Arcadia Software Limited. Copyright 2008-2010